Cardiac arrhythmias
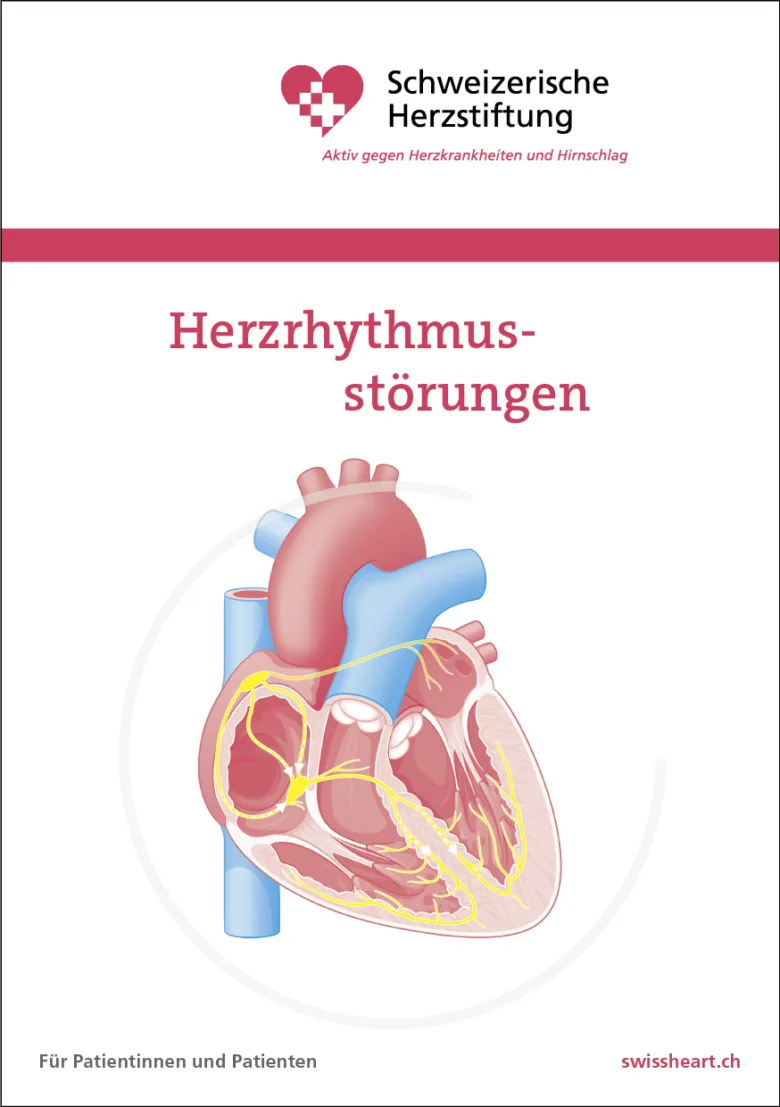
The normal heart rate is 50 to 100 beats per minute.
The variability of the heart rate, for example during excitement or physical exertion, is normal and is not in itself a cause for anxiety or concern.
Heart rhythm –
disorders
The normal heart rate is 50 to 100 beats per minute.
The variability of the heart rate, for example during excitement or physical exertion, is normal and is not in itself a cause for anxiety or concern.
- If the pulse is too slow (less than 50 beats per minute), dizziness, light-headedness or fainting may occur because of insufficient blood supply of the brain
- Tiredness, poor performance and extreme exhaustion
- Shortness of breath especially during physical exertion
- Disorder of the electrical conduction system of the heart, particularly in the sinus node (the heart’s “pacemaker”) or in the conduction pathways
- In combination with other forms of heart disease, such as heart attack, heart valve disease or inflammation
- Side effects of medication
- In athletes/younger people, a slow pulse can also represent a well-trained status and is then usually normal
- Electrocardiogram (ECG): Measures the electrical activity of the heart and is the most important examination method
- Long-term ECG: The heart rhythm is recorded over 1-7 days in order to detect even rare disturbances
- Ultrasound examination of the heart (TTE) to assess heart structure and function
- Further examinations such as blood tests or exercise ECG can help to determine the etiology
- Treatment of the underlying disease, e.g. discontinuation of medication, or specific treatment for other heart diseases
- Adjustment or discontinuation of medication that slows down the heart rate
- If the symptoms are pronounced or the pulse is very slow, a pacemaker may be necessary to regulate the heartbeat (see below)
- In rare cases, medication can be used to increase the heart rate temporarily
- Palpitations (more than 100 times per minute at rest) or an uncomfortably strong palpitation that often starts suddenly.
- Dizziness, light-headedness or the feeling of about to faint.
- Shortness of breath and shortness of breath, especially on exertion.
- Restlessness, feelings of anxiety or chest pain are possible.
Most common:
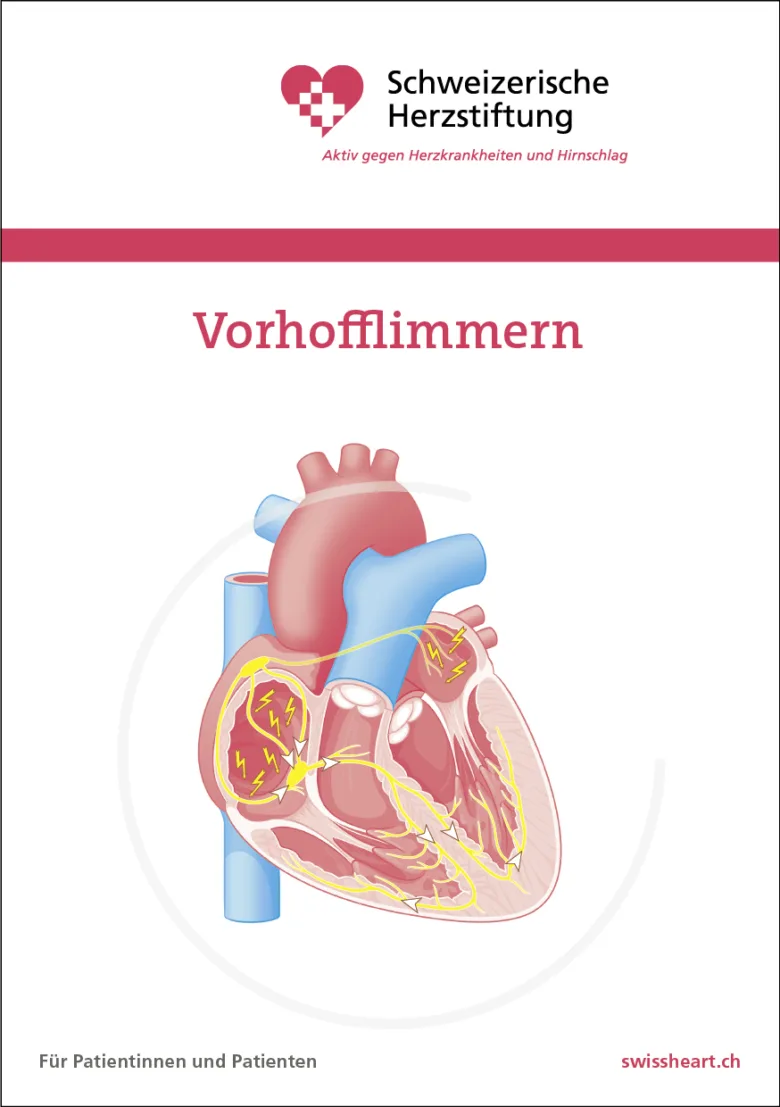
- Atrial fibrillation (irregularpulse): with increasing age and certain heart diseases
- Other tachycardias of the atrium or AV node(regularpulse): often no recognizable cause, sometimes congenital conduction disorder
- All are favored by strong physical or mental strain, stress, fever, inflammation or lack of fluids as well as electrolyte disorders and occur as side effects of medication and excessive consumption of caffeine, alcohol or drugs
Rarer:
- Ventricular tachycardia or ventricular fibrillation : During acute myocardial infarction, in all forms of myocardial disease and cardiac insufficiency. Often fatal if left untreated
- Electrocardiogram (ECG): Shows the type and origin of the cardiac arrhythmia.
- Long-term ECG (for weeks to years): Also records transient or infrequent attacks of palpitations.
- Ultrasound examination of the heart (TTE) to assess heart structure and function.
- Blood tests to rule out other causes such as hyperthyroidism or electrolyte imbalances.
- Electrophysiological clarification (cardiac catheterization, see below)
- Treatment of the underlying disease or adjustment of medication.
- Medication to control the heart rhythm and heart rate (antiarrhythmic drugs, beta blockers).
- In certain cases, electrical cardioversion (‘electric shock’ under anesthesia, to restore the normal rhythm).
- In the case of recurrent or dangerous tachycardia, a cardiac catheter procedure (ablation) or an implantable defibrillator may be necessary (see below).
- Most people do not even notice extra beats (extrasystoles) (ALL people have extrasystoles!)
- Heart stumbling or the feeling of a “skip” in the heartbeat, sometimes followed by a strong beat that can be felt in the throat
- Occasionally dizziness, nausea or a brief feeling of weakness (especially if occurring frequently)
- Anxiety, restlessness or feelings of insecurity, especially if the extrasystoles occur more frequently or at night in the left-sided position
- Extrasystoles are additional heartbeats that occur outside the normal heart rhythm. They are often perceived as “heart stumbles”
- Most common causes: stress, lack of sleep, exhaustion, excessive consumption of alcohol, caffeine, nicotine or other addictive substances
- Electrolyte disorders, especially potassium or magnesium deficiency
- Diseases of the heart, e.g. chronic narrowing of the coronary arteries, myocarditis or heart valve disease
- Thyroid diseases, side effects of medication
- Resting ECG to detect extrasystoles and assess the heart rhythm
- Long-term ECG (over 1-7 days) to detect even rare or exercise-induced extrasystoles
- Load test: Influence of the load on the occurrence of extra strokes
- Ultrasound examination of the heart (echocardiography) to clarify possible structural heart diseases
- Blood tests to check electrolytes and thyroid levels
- In the case of harmless extrasystoles, avoiding triggers such as stress, alcohol or caffeine is often sufficient
- Compensation of electrolyte deficiencies through diet or supplements (e.g. potassium, magnesium)
- Drug treatment (e.g. beta blockers) for severe symptoms or underlying heart disease
- In very rare cases, catheter ablation (sclerotherapy of the original site in the heart)
- If the pulse is too slow (less than 50 beats per minute), dizziness, light-headedness or fainting may occur because of insufficient blood supply of the brain
- Tiredness, poor performance and extreme exhaustion
- Shortness of breath especially during physical exertion
- Disorder of the electrical conduction system of the heart, particularly in the sinus node (the heart’s “pacemaker”) or in the conduction pathways
- In combination with other forms of heart disease, such as heart attack, heart valve disease or inflammation
- Side effects of medication
- In athletes/younger people, a slow pulse can also represent a well-trained status and is then usually normal
- Electrocardiogram (ECG): Measures the electrical activity of the heart and is the most important examination method
- Long-term ECG: The heart rhythm is recorded over 1-7 days in order to detect even rare disturbances
- Ultrasound examination of the heart (TTE) to assess heart structure and function
- Further examinations such as blood tests or exercise ECG can help to determine the etiology
- Treatment of the underlying disease, e.g. discontinuation of medication, or specific treatment for other heart diseases
- Adjustment or discontinuation of medication that slows down the heart rate
- If the symptoms are pronounced or the pulse is very slow, a pacemaker may be necessary to regulate the heartbeat (see below)
- In rare cases, medication can be used to increase the heart rate temporarily
- Palpitations (more than 100 times per minute at rest) or an uncomfortably strong palpitation that often starts suddenly.
- Dizziness, light-headedness or the feeling of about to faint.
- Shortness of breath and shortness of breath, especially on exertion.
- Restlessness, feelings of anxiety or chest pain are possible.
Most common:
- Atrial fibrillation (irregularpulse): with increasing age and certain heart diseases
- Other tachycardias of the atrium or AV node(regularpulse): often no recognizable cause, sometimes congenital conduction disorder
- All are favored by strong physical or mental strain, stress, fever, inflammation or lack of fluids as well as electrolyte disorders and occur as side effects of medication and excessive consumption of caffeine, alcohol or drugs
Rarer:
- Ventricular tachycardia or ventricular fibrillation : During acute myocardial infarction, in all forms of myocardial disease and cardiac insufficiency. Often fatal if left untreated
- Electrocardiogram (ECG): Shows the type and origin of the cardiac arrhythmia.
- Long-term ECG (for weeks to years): Also records transient or infrequent attacks of palpitations.
- Ultrasound examination of the heart (TTE) to assess heart structure and function.
- Blood tests to rule out other causes such as hyperthyroidism or electrolyte imbalances.
- Electrophysiological clarification (cardiac catheterization, see below)
- Treatment of the underlying disease or adjustment of medication.
- Medication to control the heart rhythm and heart rate (antiarrhythmic drugs, beta blockers).
- In certain cases, electrical cardioversion (‘electric shock’ under anesthesia, to restore the normal rhythm).
- In the case of recurrent or dangerous tachycardia, a cardiac catheter procedure (ablation) or an implantable defibrillator may be necessary (see below).
- Most people do not even notice extra beats (extrasystoles) (ALL people have extrasystoles!)
- Heart stumbling or the feeling of a “skip” in the heartbeat, sometimes followed by a strong beat that can be felt in the throat
- Occasionally dizziness, nausea or a brief feeling of weakness (especially if occurring frequently)
- Anxiety, restlessness or feelings of insecurity, especially if the extrasystoles occur more frequently or at night in the left-sided position
- Extrasystoles are additional heartbeats that occur outside the normal heart rhythm. They are often perceived as “heart stumbles”
- Most common causes: stress, lack of sleep, exhaustion, excessive consumption of alcohol, caffeine, nicotine or other addictive substances
- Electrolyte disorders, especially potassium or magnesium deficiency
- Diseases of the heart, e.g. chronic narrowing of the coronary arteries, myocarditis or heart valve disease
- Thyroid diseases, side effects of medication
- Resting ECG to detect extrasystoles and assess the heart rhythm
- Long-term ECG (over 1-7 days) to detect even rare or exercise-induced extrasystoles
- Load test: Influence of the load on the occurrence of extra strokes
- Ultrasound examination of the heart (echocardiography) to clarify possible structural heart diseases
- Blood tests to check electrolytes and thyroid levels
- In the case of harmless extrasystoles, avoiding triggers such as stress, alcohol or caffeine is often sufficient
- Compensation of electrolyte deficiencies through diet or supplements (e.g. potassium, magnesium)
- Drug treatment (e.g. beta blockers) for severe symptoms or underlying heart disease
- In very rare cases, catheter ablation (sclerotherapy of the original site in the heart)
Specific therapies for cardiac arrhythmias
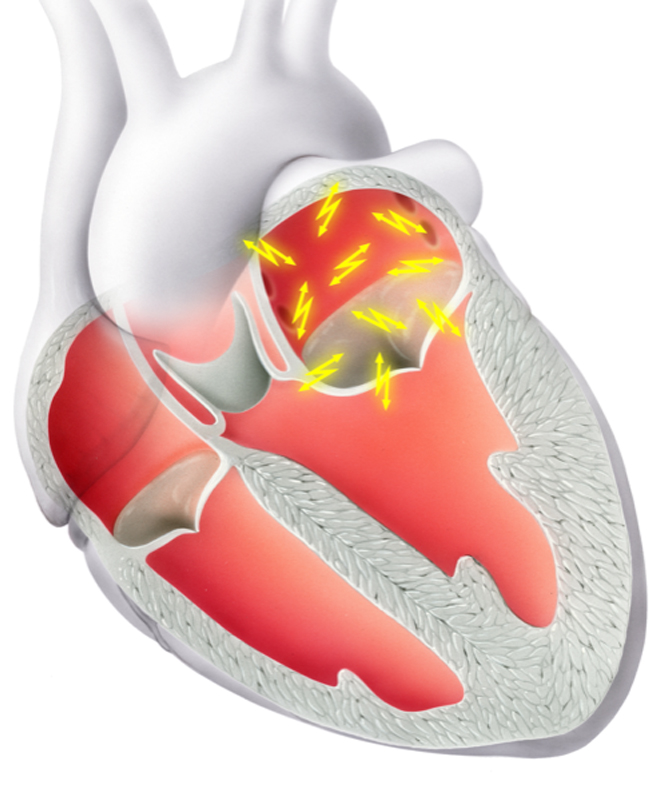
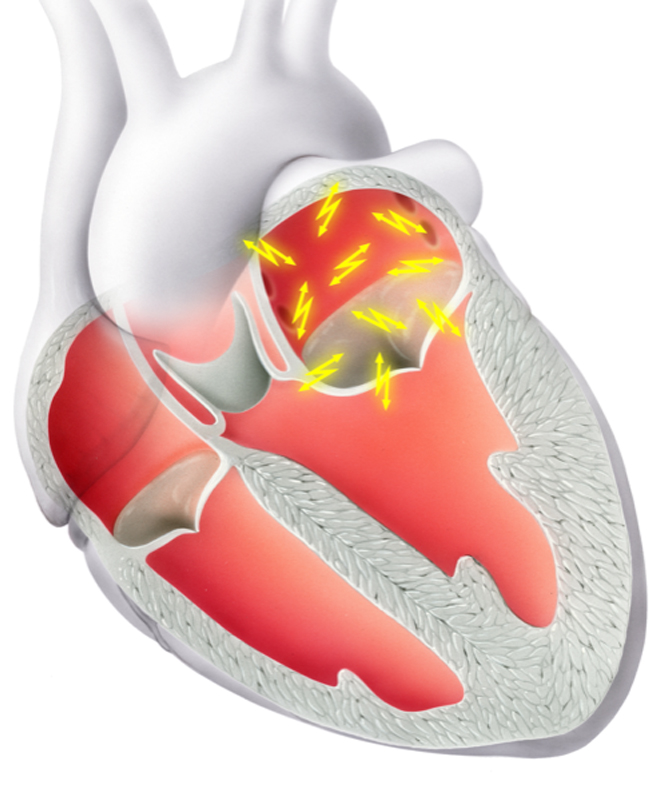
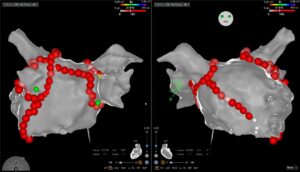
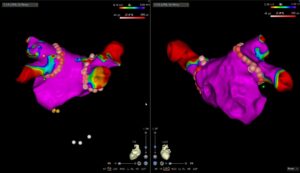
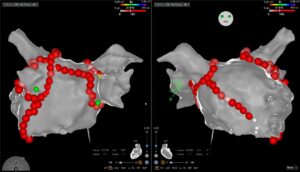
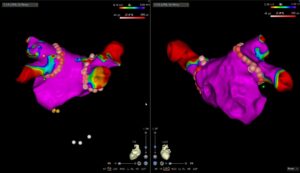
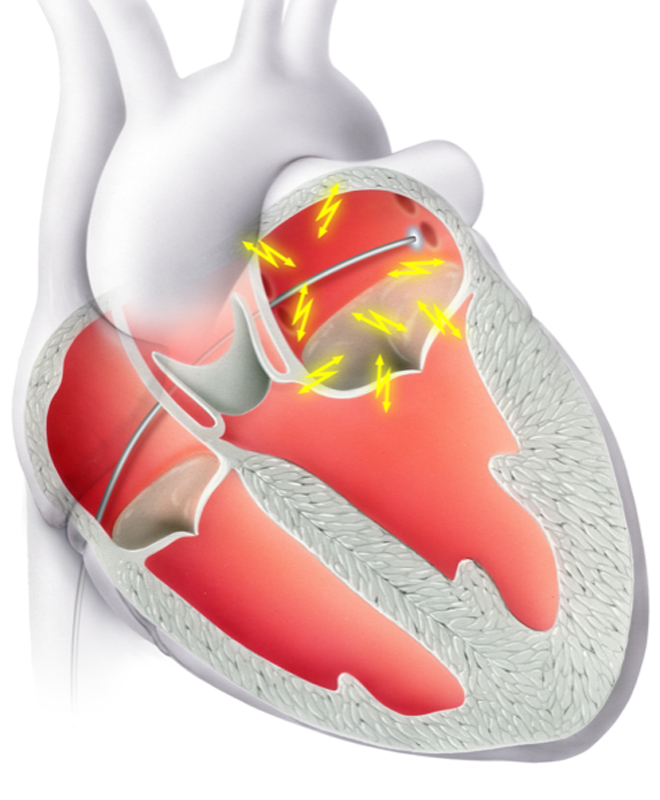 Ablation using special catheters is a proven therapy for various cardiac arrhythmias, especially if rhythm control is to be achieved. For this purpose, various regions on the inside of the heart responsible for the arrhythmia are located as part of an electrophysiological study (EPS). The tip of the electrode is then heated or cooled in order to ablate the diseased cells. The aim of the created lesions is to restrict the spread of the electrical impulses and thus eliminate the arrhythmia.
Ablation using special catheters is a proven therapy for various cardiac arrhythmias, especially if rhythm control is to be achieved. For this purpose, various regions on the inside of the heart responsible for the arrhythmia are located as part of an electrophysiological study (EPS). The tip of the electrode is then heated or cooled in order to ablate the diseased cells. The aim of the created lesions is to restrict the spread of the electrical impulses and thus eliminate the arrhythmia.
Typical cardiac arrhythmias that can be treated by ablation are
- Atrial fibrillation (Fig. 1 and 2)
- Atrial flutter
- AV node reentry tachycardia
- Wolf-Parkinson-White syndrome (WPW)
- Focal atrial tachycardia
- Ventricular extra-beats
- Ventricular tachycardia
The chance of ablation success depends on many factors, including the arrhythmia itself and any concomitant illnesses, etc. In a personal consultation, we will discuss the options available to you and draw up an individual treatment plan.
Illustrations:
Fig 1 and 2: Atrial fibrillation ablation with 3D mapping system
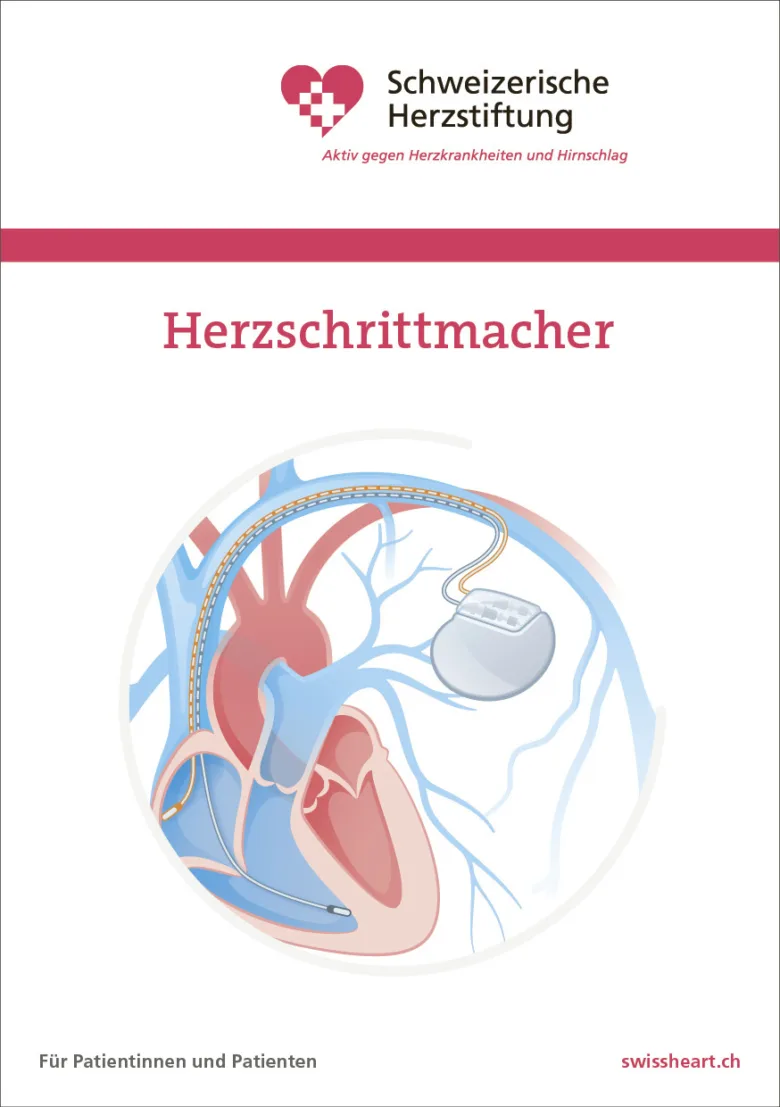
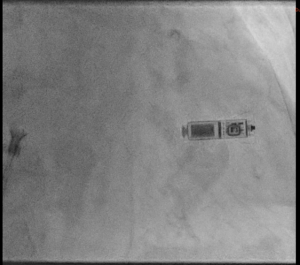
As an alternative, the so-called “electrodeless pacemaker” is available in certain situations. In this case, a small pacemaker “capsule” is implanted directly into the right ventricle via the vein in the groin. This system does not require an actual “unit” or electrodes (Fig. 3). In an individual analysis, we assess which system is best suited for which patient.
Fig 3
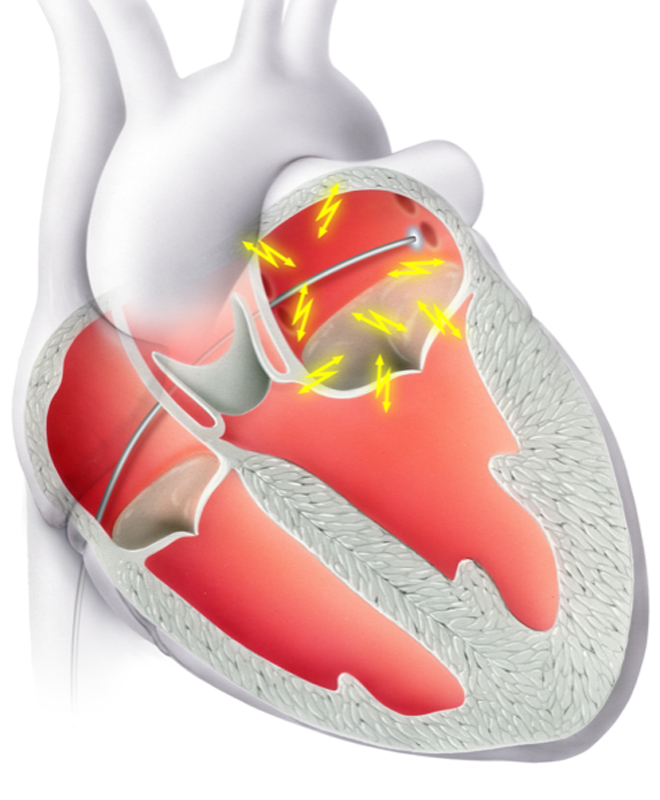
If there is a high risk of life-threatening cardiac arrhythmia, it may be necessary to implant an internal shock device (ICD). The ICD is implanted in local anesthesia in a similar way to a pacemaker.
The defibrillator continuously monitors the heart rhythm and detects a rapid and life-threatening heart rhythm. In this case, it can restore the normal heart rhythm by overstimulation or by delivering an electric shock.

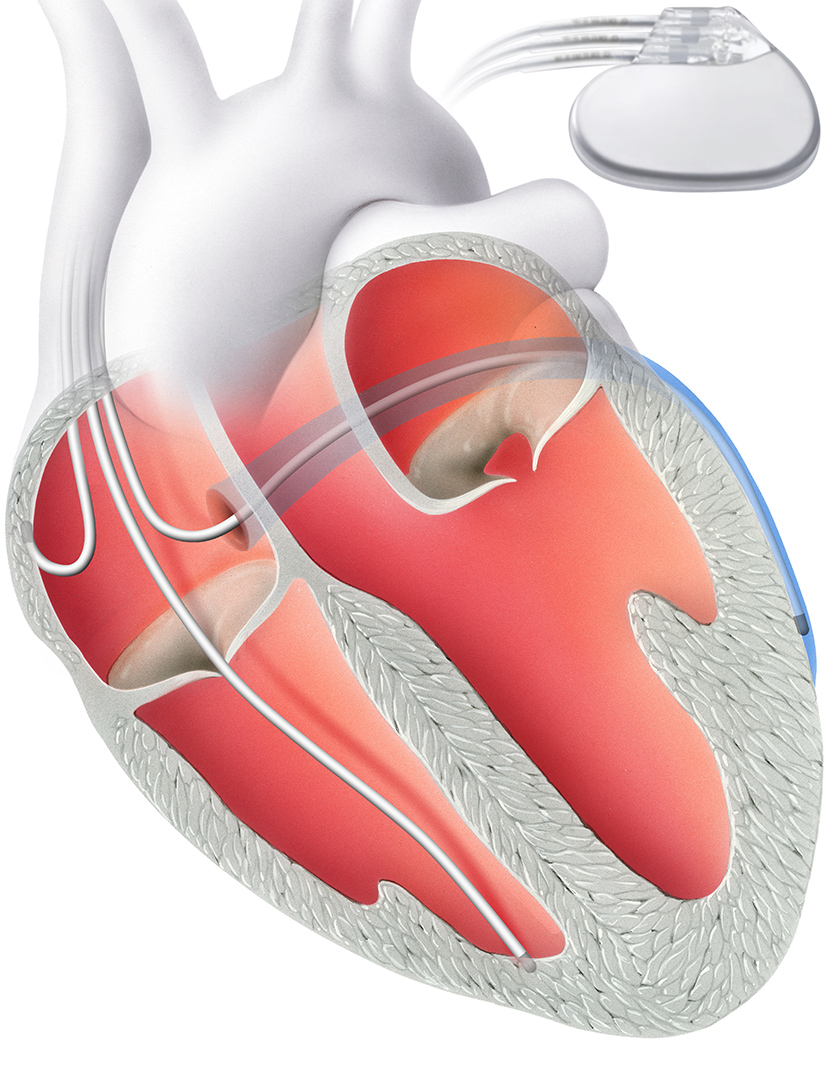
Similar to a pacemaker, the defibrillator consists of two components: Firstly, an electrode that is anchored in the right ventricle via the vein. The second is a device with a battery, which is implanted subcutaneously.
In standard ICD therapy, an electrode is implanted directly into the heart. It is part of a defibrillator that can normalize the rhythm if the heartbeat is too fast.
The subcutaneous ICD (S-ICD) has been available as an alternative for almost 10 years. With this form of therapy, the heart and blood vessels remain unaffected: an electrode is not implanted directly into the heart, but above the sternum directly under the skin (“subcutaneously”). This significantly reduces the risk of electrode complications and complications during possible electrode removal. However, the risk of so-called “inadequate shock delivery” (“misfires”) is slightly higher than with standard ICDs with electrodes in the heart.
Dyssynchrony is both a cause and a consequence of cardiac insufficiency. This means that the left and right ventricles are no longer stimulated in a synchronized mode. This dyssynchrony means that the pumping action is no longer effective and it itself enhances the cardiac insufficiency (vicious circle).
Improve synchrony
Cardiac resynchronization therapy (CRT) corrects this problem. It aims to improve the synchrony of the left and right ventricles. A biventricular pacemaker, i.e. one that stimulates both ventricles, is implanted for this purpose.
The CRT device does not have two electrodes like a conventional pacemaker, but three. The additional electrode is inserted into a coronary vein in front of the left ventricle. Alternatively, it can be inserted via a thoracoscopic approach, a minimal incision in the chest.
Thanks to this third electrode, it is possible to stimulate both ventricles at the same time. A hospital stay of two to three days is required for the procedure.
Implantation loop recorders are used to record cardiac arrhythmias in the event of unconsciousness for which no cause has yet been found or for long-term monitoring of the heart rhythm. An event recorder is usually combined with remote monitoring. An ECG is automatically saved in the event of special events (unconsciousness, arrhythmia).
The procedure is performed in local anesthesia and on an outpatient basis. The recorder is implanted subcutaneously in the area of the left rib cage through a small incision in the skin.
Ablation using special catheters is a proven therapy for various cardiac arrhythmias, especially if rhythm control is to be achieved. For this purpose, various regions on the inside of the heart responsible for the arrhythmia are located as part of an electrophysiological study (EPS). The tip of the electrode is then heated or cooled in order to ablate the diseased cells. The aim of the created lesions is to restrict the spread of the electrical impulses and thus eliminate the arrhythmia.
Typical cardiac arrhythmias that can be treated by ablation are
- Atrial fibrillation (Fig. 1 and 2)
- Atrial flutter
- AV node reentry tachycardia
- Wolf-Parkinson-White syndrome (WPW)
- Focal atrial tachycardia
- Ventricular extra-beats
- Ventricular tachycardia
The chance of ablation success depends on many factors, including the arrhythmia itself and any concomitant illnesses, etc. In a personal consultation, we will discuss the options available to you and draw up an individual treatment plan.
Illustrations:
Fig 1 and 2: Atrial fibrillation ablation with 3D mapping system
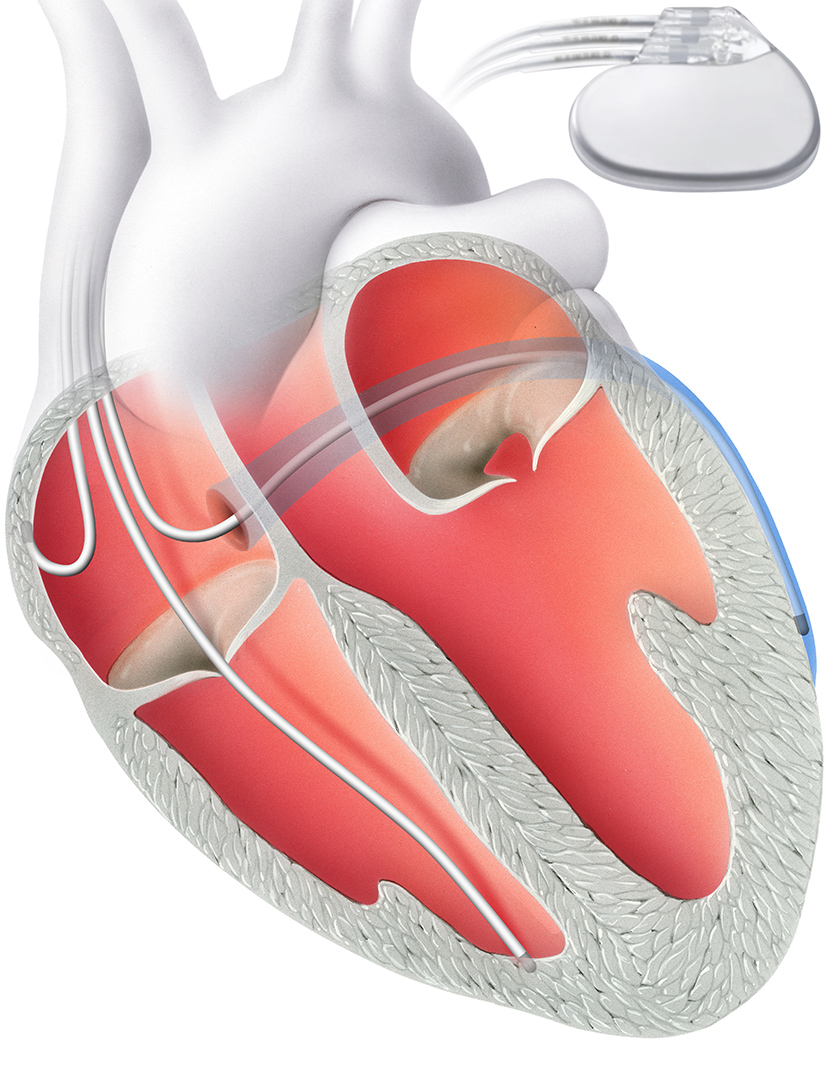
The pacemaker is implanted subcutaneously in local anesthesia in an operation lasting just under an hour. The electrodes are inserted into a vein and anchored in the ventricle under X-ray control. Electrical impulses are emitted via the electrode to stimulate the heart and thus increase the heart rate. The individually programmable pacemaker is usually checked once or twice a year.
As an alternative, the so-called “electrodeless pacemaker” is available in certain situations. In this case, a small pacemaker “capsule” is implanted directly into the right ventricle via the vein in the groin. This system does not require an actual “unit” or electrodes (Fig. 3). In an individual analysis, we assess which system is best suited for which patient.
Fig 3
If there is a high risk of life-threatening cardiac arrhythmia, it may be necessary to implant an internal shock device (ICD). The ICD is implanted in local anesthesia in a similar way to a pacemaker.
The defibrillator continuously monitors the heart rhythm and detects a rapid and life-threatening heart rhythm. In this case, it can restore the normal heart rhythm by overstimulation or by delivering an electric shock.

Similar to a pacemaker, the defibrillator consists of two components: Firstly, an electrode that is anchored in the right ventricle via the vein. The second is a device with a battery, which is implanted subcutaneously.
In standard ICD therapy, an electrode is implanted directly into the heart. It is part of a defibrillator that can normalize the rhythm if the heartbeat is too fast.
The subcutaneous ICD (S-ICD) has been available as an alternative for almost 10 years. With this form of therapy, the heart and blood vessels remain unaffected: an electrode is not implanted directly into the heart, but above the sternum directly under the skin (“subcutaneously”). This significantly reduces the risk of electrode complications and complications during possible electrode removal. However, the risk of so-called “inadequate shock delivery” (“misfires”) is slightly higher than with standard ICDs with electrodes in the heart.
Dyssynchrony is both a cause and a consequence of cardiac insufficiency. This means that the left and right ventricles are no longer stimulated in a synchronized mode. This dyssynchrony means that the pumping action is no longer effective and it itself enhances the cardiac insufficiency (vicious circle).
Improve synchrony
Cardiac resynchronization therapy (CRT) corrects this problem. It aims to improve the synchrony of the left and right ventricles. A biventricular pacemaker, i.e. one that stimulates both ventricles, is implanted for this purpose.
The CRT device does not have two electrodes like a conventional pacemaker, but three. The additional electrode is inserted into a coronary vein in front of the left ventricle. Alternatively, it can be inserted via a thoracoscopic approach, a minimal incision in the chest.
Thanks to this third electrode, it is possible to stimulate both ventricles at the same time. A hospital stay of two to three days is required for the procedure.
Implantation loop recorders are used to record cardiac arrhythmias in the event of unconsciousness for which no cause has yet been found or for long-term monitoring of the heart rhythm. An event recorder is usually combined with remote monitoring. An ECG is automatically saved in the event of special events (unconsciousness, arrhythmia).
The procedure is performed in local anesthesia and on an outpatient basis. The recorder is implanted subcutaneously in the area of the left rib cage through a small incision in the skin.
Further information
Our specialists for cardiac arrhythmias

PD Dr. med.
PD Dr. med.
David Hürlimann
David Hürlimann
Cardiology | Rhythmology
Cardiology | Rhythmology
DE – EN – FR
DE – EN – FR

Dr. med.
Dr. med.
Luca Oechslin
Luca Oechslin
Senior physician cardiology
Senior physician cardiology
DE – EN – IT
DE – EN – IT