Heart failure
Heart failure (medically known as ‘heart failure’) stands for the inability of the heart muscle to pump enough blood to the various organs.
Heart failure can have many different causes. Typical symptoms include tiredness, reduced workout capacity, shortness of breath, lack of appetite and swollen legs.
Heart failure
Heart failure (medically known as ‘heart failure’) stands for the inability of the heart muscle to pump enough blood to the various organs.
Heart failure can have many different causes. Typical symptoms include tiredness, reduced workout capacity, shortness of breath, lack of appetite and swollen legs.
The symptoms of heart failure can be very unspecific, such as fatigue or decreasing workout capacity. Cardiac arrhythmias also occur more frequently. Depending on the side of the heart is primarily affected, other symptoms may also occur:
Left side of heart failure:
- Shortness of breath on exertion, when speaking or even at rest
- Discomfort when lying flat (upper body elevation necessary)
- Dizziness
Right side of heart failure:
- Decreased appetite with abdominal discomfort and loss of appetite
- Swelling of the legs/lower legs/ankles
- Declining workout capacity
Heart failure can be the result of various conditions, including valvular heart disease, coronary artery disease, arrhythmias, high blood pressure or a combination of several conditions.
However, it can also develop primarily as a heart muscle disease. Furthermore, it can be the result of congenital heart disease or diseases of other organs. In addition, external factors such as infections, radiation and drug treatments (especially chemotherapy) can also lead to heart failure.
Since a variety of problems can ultimately lead to heart failure, a combination of tests as listed below are often necessary:
- Assessment of symptoms and medical history
- Physical examination incl. blood pressure measurement
- Resting ECG
- Exercise ECG
- Blood tests on various organ systems (heart, liver, kidneys, infections…)
- Cardiac ultrasound examination
- Heart MRI
- CT of the coronary arteries
- Cardiac catheter examinations
- Heart muscle biopsy
We distinguish between general and specific therapies.
General therapies:
- Optimization of risk factors:
- Nutritional optimization
- Weight reduction (with/without medication)
- Smoking cessation
- increase physical activity
- Blood pressure and diabetes control
- Treatment of iron deficiency
- drug treatment:
- diuretic medication
- Medication against cardiac arrhythmia
- specific heart failure medication
- Inhibitors of the renin-angiotensin-aldosterone system (ACE inhibitors, sartans, sacubitril-valsartan, aldosterone receptor antagonists)
- SGLT2 inhibitors
Specific therapies:
- Treatment of the underlying problem (e.g. replacement of a narrow or leaking heart valve, treatment of blocked coronary arteries, elimination of arrhythmia, etc., see the ‘Therapy’ section for the respective heart disease)
- Cardiac resynchronization therapy (see below)
- Implantation of a defibrillator (see below)
- LVAD – left ventricular assist devices
- Heart transplantation
The symptoms of heart failure can be very unspecific, such as fatigue or decreasing workout capacity. Cardiac arrhythmias also occur more frequently. Depending on the side of the heart is primarily affected, other symptoms may also occur:
Left side of heart failure:
- Shortness of breath on exertion, when speaking or even at rest
- Discomfort when lying flat (upper body elevation necessary)
- Dizziness
Right side of heart failure:
- Decreased appetite with abdominal discomfort and loss of appetite
- Swelling of the legs/lower legs/ankles
- Declining workout capacity
Heart failure is the end stage of various heart diseases that could not be treated in time or effectively.
Heart failure can be the result of various conditions, including valvular heart disease, coronary artery disease, arrhythmias, high blood pressure or a combination of several conditions.
However, it can also develop primarily as a heart muscle disease. Furthermore, it can be the result of congenital heart disease or diseases of other organs. In addition, external factors such as infections, radiation and drug treatments (especially chemotherapy) can also lead to heart failure.
Since a variety of problems can ultimately lead to heart failure, a combination of tests as listed below are often necessary:
- Assessment of symptoms and medical history
- Physical examination incl. blood pressure measurement
- Resting ECG
- Exercise ECG
- Blood tests on various organ systems (heart, liver, kidneys, infections…)
- Cardiac ultrasound examination
- Heart MRI
- CT of the coronary arteries
- Cardiac catheter examinations
- Heart muscle biopsy
We distinguish between general and specific therapies.
General therapies:
- Optimization of risk factors:
- Nutritional optimization
- Weight reduction (with/without medication)
- Smoking cessation
- increase physical activity
- Blood pressure and diabetes control
- Treatment of iron deficiency
- drug treatment:
- diuretic medication
- Medication against cardiac arrhythmia
- specific heart failure medication
- Inhibitors of the renin-angiotensin-aldosterone system (ACE inhibitors, sartans, sacubitril-valsartan, aldosterone receptor antagonists)
- SGLT2 inhibitors
Specific therapies:
- Treatment of the underlying problem (e.g. replacement of a narrow or leaking heart valve, treatment of blocked coronary arteries, elimination of arrhythmia, etc., see the ‘Therapy’ section for the respective heart disease)
- Cardiac resynchronization therapy (see below)
- Implantation of a defibrillator (see below)
- LVAD – left ventricular assist devices
- Heart transplantation
Specific therapies for heart failure
Dyssynchrony is both a cause and a consequence of heart failure. This means that the left and right ventricles are no longer stimulated to beat at the same time, but at different times. This dyssynchrony means that the pumping action is no longer effective and it itself exacerbates the heart failure (vicious circle).
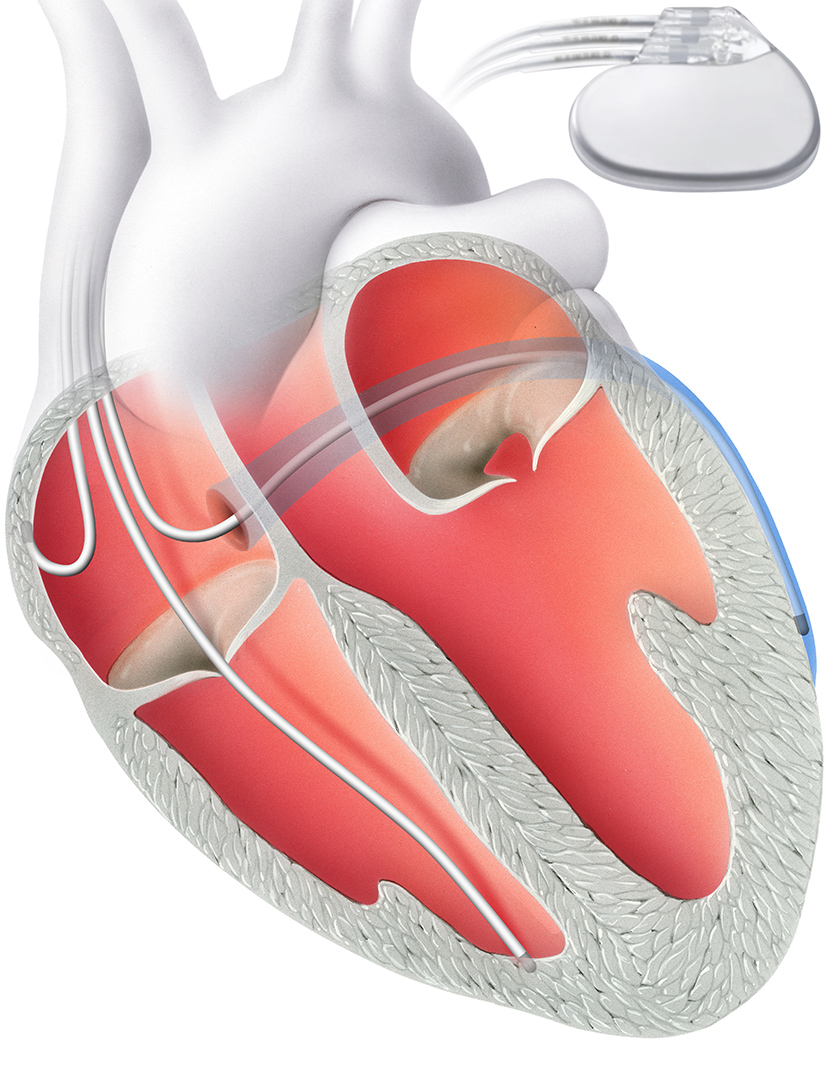
Improve synchrony
Cardiac resynchronization therapy (CRT) corrects this problem. It aims to improve the synchrony of the left and right ventricles. A biventricular pacemaker, i.e. one that stimulates both ventricles, is implanted for this purpose.
This does not have two electrodes like a conventional pacemaker, but three. The additional electrode is inserted into a coronary vein in front of the left ventricle. Alternatively, it can be inserted via a thoracoscopic approach, a minimal incision in the chest.
Thanks to this third electrode, it is possible to stimulate both ventricles at the same time. A hospital stay of two to three days is required for the procedure.
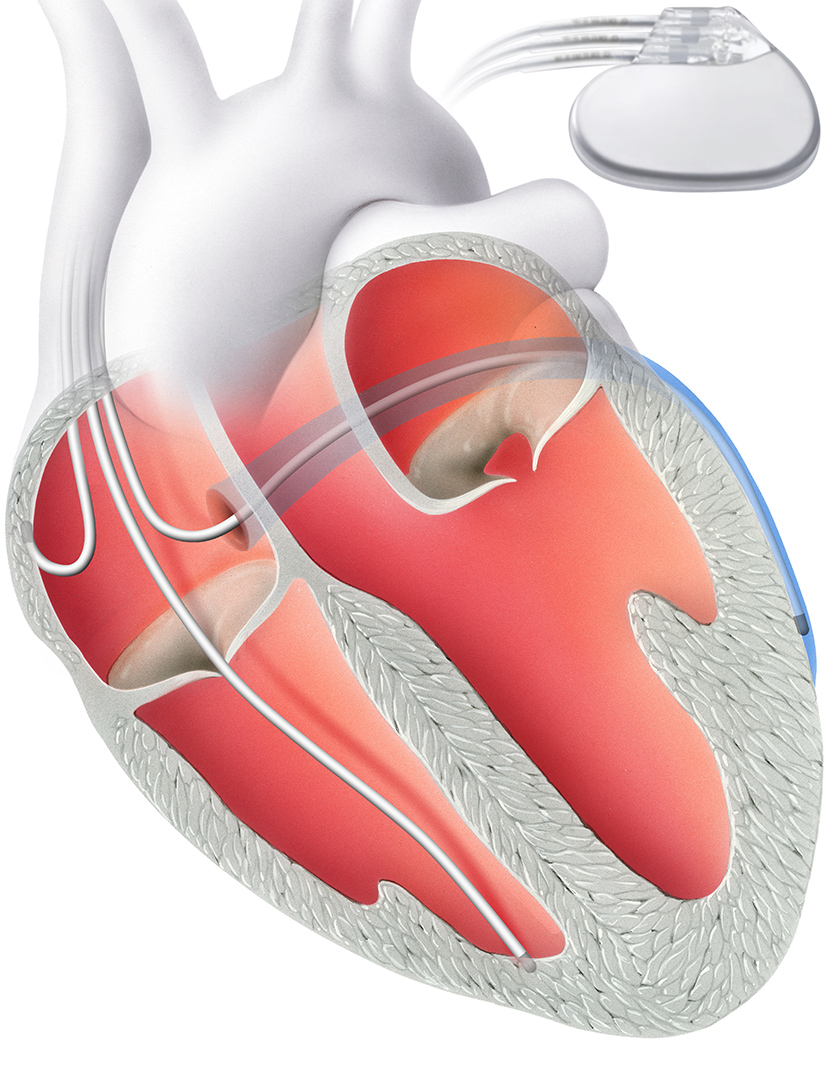
If there is a high risk of life-threatening cardiac arrhythmia, it may be necessary to implant an internal shock device (ICD). The ICD is implanted under local anesthesia in a similar way to a pacemaker.
The defibrillator continuously monitors the heart rhythm and detects a rapid and life-threatening heart rhythm. In this case, it can restore the normal heart rhythm by overstimulation or by delivering an electric shock.

Similar to a pacemaker, the defibrillator consists of two components: Firstly, an electrode that is anchored in the right ventricle via the vein. The second is a device with a battery, which is implanted under the skin.
In standard ICD therapy, an electrode is implanted directly into the heart. It is part of a defibrillator that can normalize the rhythm if the heartbeat is too fast.
The subcutaneous ICD (S-ICD) has been available as an alternative for almost 10 years. With this form of therapy, the heart and blood arteries remain unaffected: an electrode is not implanted directly into the heart, but above the sternum directly under the skin (“subcutaneously”). This significantly reduces the risk of electrode complications and complications during possible electrode removal. However, the risk of so-called “inadequate shock delivery” (“misfires”) is slightly higher than with standard ICDs with electrodes in the heart.
Dyssynchrony is both a cause and a consequence of heart failure. This means that the left and right ventricles are no longer stimulated to beat at the same time, but at different times. This dyssynchrony means that the pumping action is no longer effective and it itself exacerbates the heart failure (vicious circle).
Improve synchrony
Cardiac resynchronization therapy (CRT) corrects this problem. It aims to improve the synchrony of the left and right ventricles. A biventricular pacemaker, i.e. one that stimulates both ventricles, is implanted for this purpose.
This does not have two electrodes like a conventional pacemaker, but three. The additional electrode is inserted into a coronary vein in front of the left ventricle. Alternatively, it can be inserted via a thoracoscopic approach, a minimal incision in the chest.
Thanks to this third electrode, it is possible to stimulate both ventricles at the same time. A hospital stay of two to three days is required for the procedure.
If there is a high risk of life-threatening cardiac arrhythmia, it may be necessary to implant an internal shock device (ICD). The ICD is implanted under local anesthesia in a similar way to a pacemaker.
The defibrillator continuously monitors the heart rhythm and detects a rapid and life-threatening heart rhythm. In this case, it can restore the normal heart rhythm by overstimulation or by delivering an electric shock.

Similar to a pacemaker, the defibrillator consists of two components: Firstly, an electrode that is anchored in the right ventricle via the vein. The second is a device with a battery, which is implanted under the skin.
In standard ICD therapy, an electrode is implanted directly into the heart. It is part of a defibrillator that can normalize the rhythm if the heartbeat is too fast.
The subcutaneous ICD (S-ICD) has been available as an alternative for almost 10 years. With this form of therapy, the heart and blood arteries remain unaffected: an electrode is not implanted directly into the heart, but above the sternum directly under the skin (“subcutaneously”). This significantly reduces the risk of electrode complications and complications during possible electrode removal. However, the risk of so-called “inadequate shock delivery” (“misfires”) is slightly higher than with standard ICDs with electrodes in the heart.
Further information
Our specialists for heart failure
ICD

Prof. Dr. med.
Prof. Dr. med.
Jürg Grünenfelder
Jürg Grünenfelder
Cardiac surgery
Cardiac surgery
DE – EN – IT – FR
DE – EN – IT – FR
CRT & ICD

PD Dr. med.
PD Dr. med.
David Hürlimann
David Hürlimann
Cardiology | Rhythmology
Cardiology | Rhythmology
DE – EN – FR
DE – EN – FR
Heart failure

Prof. Dr. med.
Prof. Dr. med.
Georg Noll
Georg Noll
Cardiology | Prevention
Cardiology | Prevention
DE – EN – FR – IT
DE – EN – FR – IT
CRT & ICD