Aortic diseases
The aorta (main artery) increases in size over the course of a lifetime. If this enlargement exceeds a normal level, we speak of dilatation or even aneurysm (severe enlargement).
Tearing of the wall layers of the aorta (aortic dissection) is a life-threatening emergency and must be treated immediately.
Aortic diseases
The aorta (main artery) increases in size over the course of a lifetime. If this enlargement exceeds a normal level, we speak of dilatation or even aneurysm (severe enlargement).
Tearing of the wall layers of the aorta (aortic dissection) is a life-threatening emergency and must be treated immediately.
- Usually no complaints
- With large expansion: feeling of pressure or pain in the chest, occasionally back pain
- Rarely: Shortness of breath, hoarseness or difficulty swallowing due to pressure on neighboring structures such as nerves or the esophagus
- Age-related changes and wear and tear of the vessel wall (degradation processes)
- Uncontrolled high blood pressure (most common risk factor)
- Congenital connective tissue diseases: Marfan syndrome, Loeys-Dietz syndrome, Ehlers-Danlos syndrome, familial non-syndromic thoracic aortic aneurysms, in the context of bicuspid aortic valve, as well as many other as yet unrecognized genetic forms
- Rarer: inflammation or consequences of infections
- Often an incidental finding during ultrasound examinations (echocardiography) or X-rays
- Transthoracic echocardiography (TTE) for initial and follow-up examinations and screening of relatives
- Computed tomography (CT) or magnetic resonance imaging (MRI) for exact size determination and expansion as well as for follow-up checks
- Regular cardiological checks in the event of minor dilatation to monitor the size
- Treatment of risk factors, in particular optimal blood pressure control
- Surgery with replacement of the affected section if the aneurysm reaches a critical size (usually from 5.0-5.5 cm, depending on the case) or causes discomfort
- In special cases, early surgery for genetic or uncontrollable risk factors, corresponding family history or rapid size increase
- Sudden, very strong, tearing or stabbing pain in the chest, often also moving into the back between the shoulder blades or the abdomen
- Loss of consciousness or dizziness or even fainting
- Tingling, pain or paralysis in the limbs or face (like a stroke)
- Shortness of breath
- Congenital connective tissue diseases such as Marfan, Loeys-Dietz or Ehlers-Danlos syndrome
- Pre-existing idiopathic or familial aneurysms of the aorta
- Vascular inflammation or injuries (e.g. due to accidents with high braking force)
- Uncontrolled high blood pressure (hypertension) and severe arteriosclerosis (vascular calcification)
- Very rare: Complications after surgery or cardiac catheterization and at the end of pregnancy
- Typical medical history (previous history and acute event)
- Clinical examination (pulse status and blood pressure differences, auscultation)
- Emergency computed tomography (CT) of the entire aorta
- ECG and ultrasound examinations help to rule out other causes such as a heart attack and to assess the aorta, the aortic valve and the heart function
- Blood tests to rule out concomitant diseases or organ damage
- Immediate emergency treatment, usually in an intensive care unit or operating theater
- In type A (dissection close to the heart: aortic root and ascending aorta also affected): Emergency surgery to stabilize the aorta and restore blood flow
- Type B (descending aorta only): monitoring, blood pressure reduction and pain therapy, surgery only in case of complications
- Long-term control and treatment of risk factors such as high blood pressure, regular follow-up examinations
- Usually no complaints
- With large expansion: feeling of pressure or pain in the chest, occasionally back pain
- Rarely: Shortness of breath, hoarseness or difficulty swallowing due to pressure on neighboring structures such as nerves or the esophagus
- Age-related changes and wear and tear of the vessel wall (degradation processes)
- Uncontrolled high blood pressure (most common risk factor)
- Congenital connective tissue diseases: Marfan syndrome, Loeys-Dietz syndrome, Ehlers-Danlos syndrome, familial non-syndromic thoracic aortic aneurysms, in the context of bicuspid aortic valve, as well as many other as yet unrecognized genetic forms
- Rarer: inflammation or consequences of infections
- Often an incidental finding during ultrasound examinations (echocardiography) or X-rays
- Transthoracic echocardiography (TTE) for initial and follow-up examinations and screening of relatives
- Computed tomography (CT) or magnetic resonance imaging (MRI) for exact size determination and expansion as well as for follow-up checks
- Regular cardiological checks in the event of minor dilatation to monitor the size
- Treatment of risk factors, in particular optimal blood pressure control
- Surgery with replacement of the affected section if the aneurysm reaches a critical size (usually from 5.0-5.5 cm, depending on the case) or causes discomfort
- In special cases, early surgery for genetic or uncontrollable risk factors, corresponding family history or rapid size increase
- Sudden, very strong, tearing or stabbing pain in the chest, often also moving into the back between the shoulder blades or the abdomen
- Loss of consciousness or dizziness or even fainting
- Tingling, pain or paralysis in the limbs or face (like a stroke)
- Shortness of breath
- Congenital connective tissue diseases such as Marfan, Loeys-Dietz or Ehlers-Danlos syndrome
- Pre-existing idiopathic or familial aneurysms of the aorta
- Vascular inflammation or injuries (e.g. due to accidents with high braking force)
- Uncontrolled high blood pressure (hypertension) and severe arteriosclerosis (vascular calcification)
- Very rare: Complications after surgery or cardiac catheterization and at the end of pregnancy
- Typical medical history (previous history and acute event)
- Clinical examination (pulse status and blood pressure differences, auscultation)
- Emergency computed tomography (CT) of the entire aorta
- ECG and ultrasound examinations help to rule out other causes such as a heart attack and to assess the aorta, the aortic valve and the heart function
- Blood tests to rule out concomitant diseases or organ damage
- Immediate emergency treatment, usually in an intensive care unit or operating theater
- In type A (dissection close to the heart: aortic root and ascending aorta also affected): Emergency surgery to stabilize the aorta and restore blood flow
- Type B (descending aorta only): monitoring, blood pressure reduction and pain therapy, surgery only in case of complications
- Long-term control and treatment of risk factors such as high blood pressure, regular follow-up examinations
Surgical therapies of the aorta
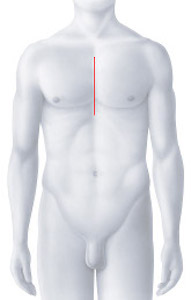
In a composite graft operation on the aortic root, both the diseased aortic valve and the enlarged aortic root are replaced with a special vascular prosthesis with an integrated artificial heart valve. Either a mechanical (double-leaflet prosthesis) or a biological prosthesis (made from sterilized pericardial tissue from pigs or cattle) can be chosen as the valve replacement. We consult patients on which prosthesis best matches their needs and expectations (the decision will depend on your age, lifestyle, and any other medical conditions you may have). During the operation, the coronary arteries are carefully separated from the old aortic root and sutured into the new vascular prosthesis to ensure that blood continues to flow to the heart. Access to the heart is usually gained via a median sternotomy, in which the sternum is opened in the middle.
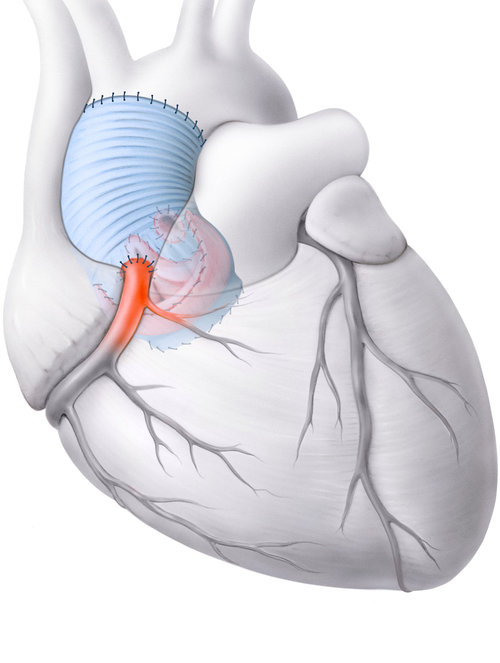
The “David operation” was named after the inventor of the procedure, the Brazilian heart surgeon Tirone Esperidiao David (1944), who worked for decades in Toronto (Canada). A valve-preserving aortic root replacement operation (Tirone David operation) is performed if the dilation of the aortic valve base (root) causes leakage of the aortic valve but the valvular cusps themselves are not pathologically altered, and if the aortic valve per se still functions normally and therefore does not need to be replaced.
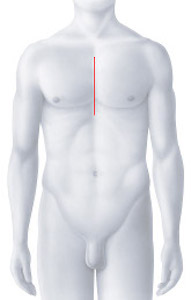
In this procedure, a vascular prosthesis is sutured in place of the enlarged aortic root. In contrast to composite graft surgery, this technique offers the possibility of preserving the natural (native) aortic valve and reconstructing it if necessary. During the operation, the coronary arteries are carefully separated from the old aortic root and sutured into the new vascular prosthesis so that blood flow to the heart is still guaranteed. This operation is performed via a median sternotomy (splitting of the sternum).
This procedure effectively prevents the risk of rupture or dissection of the ascending aorta. In supracoronary replacement of the aneurysmatic ascending aorta, only the diseased section of the aorta is replaced with a vascular prosthesis, while the aortic valve is preserved. The vascular prosthesis is sutured above the branches of the coronary arteries so that these do not need to be reconnected. Access to the heart is usually gained via a median sternotomy, in which the sternum is opened in the middle.
In a combined replacement of the aortic root and ascending aorta, both the diseased aortic valve and aortic root as well as the aneurysmal section of the ascending aorta are replaced with a vascular prosthesis with an integrated heart valve. Either a mechanical (double-leaflet prosthesis) or a biological prosthesis (made from sterilized pericardial tissue from pigs or cattle) can be chosen as the valve replacement. We consult patients on which prosthesis best matches their needs and expectations (the decision will depend on your age, lifestyle, and any other illnesses you may have). During the operation, the coronary arteries are separated from the old aortic root and sutured into the vascular prosthesis to ensure blood flow to the heart. Access to the heart is usually gained via a median sternotomy, in which the sternum is opened in the middle.
Access to the heart is usually gained via a median sternotomy, in which the sternum is opened in the middle.
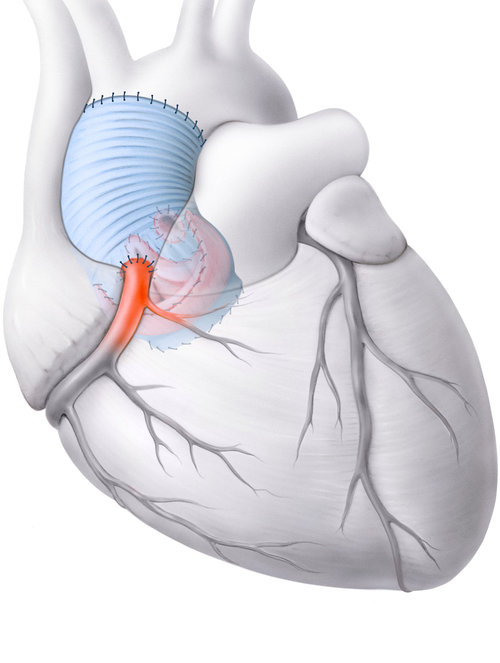
The “Tirone David operation” was named after the inventor of the procedure, the Brazilian heart surgeon Tirone Esperidiao David (1944), who worked for decades in Toronto (Canada). A valve-preserving aortic root replacement operation (Tirone David operation) is performed if the dilation of the aortic valve base (root) causes leakage of the aortic valve but the valvular cusps themselves are not pathologically altered, and if the aortic valve per se still functions normally and therefore does not need to be replaced.
In this procedure, a vascular prosthesis is sutured in place of the enlarged aortic root. In contrast to composite graft surgery, this technique offers the possibility of preserving the natural (native) aortic valve and reconstructing it if necessary. During the operation, the coronary arteries are carefully separated from the old aortic root and sutured into the new vascular prosthesis so that blood flow to the heart is still guaranteed. This operation is performed via a median sternotomy (splitting of the sternum).
The vascular prosthesis is sutured above the branches of the coronary arteries so that these do not need to be reconnected.
Access to the heart is usually gained via a median sternotomy, in which the sternum is opened in the middle.
In a combined replacement of the aortic root and ascending aorta, both the diseased aortic valve and aortic root as well as the aneurysmal section of the ascending aorta are replaced with a vascular prosthesis with an integrated heart valve. Either a mechanical (double-leaflet prosthesis) or a biological prosthesis (made from sterilized pericardial tissue from pigs or cattle) can be chosen as the valve replacement. We consult patients on which prosthesis best matches their needs and expectations (the decision will depend on your age, lifestyle, and any other illnesses you may have). During the operation, the coronary arteries are separated from the old aortic root and sutured into the vascular prosthesis to ensure blood flow to the heart.
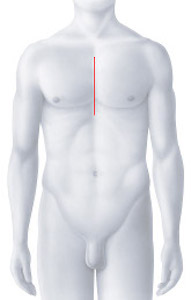
Access to the heart is usually gained via a median sternotomy, in which the sternum is opened in the middle.
Our specialists for aortic deseases

Prof. Dr. med.
Prof. Dr. med.
Patric Biaggi
Patric Biaggi
Cardiology | Imaging
Cardiology | Imaging
DE – EN – FR – IT
DE – EN – FR – IT

Graduate doctor
Graduate doctor
Daniel Fritschi
Daniel Fritschi
Senior physician cardiology
Senior physician cardiology
DE – EN
DE – EN

Prof. Dr. med.
Prof. Dr. med.
Jürg Grünenfelder
Jürg Grünenfelder
Cardiac surgery
Cardiac surgery
DE – EN – IT – FR
DE – EN – IT – FR